A leading neuroscientist is using our Cool Joints+ supplement to investigate whether its key ingredient could help people suffering with anorexia nervosa. But how could a supplement designed for joint health help with one of the UK’s most serious mental health challenges?
Dr Samantha Brooks, Associate Professor of Cognitive Neuroscience at Liverpool John Moores University, has spent over two decades studying the brain processes behind eating disorders like anorexia and bulimia.
In what would turn out to be a bittersweet twist of fate, Samantha also became an expert on Boswellia – the major ingredient in Cool Joints+ – after her dad was diagnosed with colon cancer in 2017.
“My defence mechanism was to go on PubMed and find all the things that I could ‘prescribe’ to help him, as a non-medical doctor,” says Samantha. “You do that for the people you love; you try and find out what you can.”
Boswellia, also known as Indian Frankincense, is a resin extract taken from the bark of the Boswellia serrata tree, native to India, Africa, and the Arabian Peninsula. The resin is rich in acids that have been used for centuries in traditional medicine to treat inflammation. Some studies have also found that boswellic acids may inhibit cancer growth.
Sadly, Samantha’s dad passed away in 2020. But during her research, she discovered tantalising clues that Boswellia might offer a way to support people suffering from eating disorders.
The rising risk of eating disorders in young people
Eating disorders are among the most serious mental health conditions in the UK. Anorexia nervosa, in particular, has the highest mortality rate of any psychiatric disorder, and cases are steeply on the rise – especially among adolescents and young adults.
One in eight 17-19-year olds and nearly 21% of young women were identified to have an eating disorder in a 2023 NHS mental health survey, with rates four times higher among young women than young men.
“Eating disorders like anorexia tend to occur from around the age of 13 onwards, and the core symptoms are in response to anxiety,” explains Samantha.
One of the most common triggers is social anxiety. “When you go out into the big, wide world, are you going to be attacked or accepted? Fears about fitting in are worse now, with influencers and social media.” For young women and girls, fears about unwanted sexual attention are also a major trigger.
The core symptoms of anorexia are hypervigilance – a state of heightened alertness to potential threats – and attention to detail. “You also see perfectionism, intolerance of uncertainty… things like that, especially during adolescence.”
Samantha’s research has focused on trying to identify what is happening in the brains of people with anorexia. During her PhD at King’s College in London, Samantha looked at functional magnetic resonance imaging (fMRI) scans of adults with chronic anorexia in an attempt to link the symptoms with brain processes, in the first study of its kind.
Neuroinflammation could be a hidden driver of chronic anorexia
Since then, her research has focused on the idea that a hidden driver of chronic anorexia nervosa is inflammation in the brain, driven by chronic anxiety and stress.
“When you're stressed, the hypothalamus will immediately turn off non-essential systems like appetite,” explains Samantha. “Because while you're running away from a tiger, you can't sit down and have a hamburger.”
The immune system also releases inflammatory molecules called cytokines, which spread through the body to alert that there’s a threat – whether it’s physical or perceived.
Although the brain is protected by the blood-brain barrier, some cytokines can pass through – especially near the hypothalamus – and over time, chronic exposure can lead to neuroinflammation.
“The subjective experience of inflammation is anxiety. The higher the cytokines, the higher the anxiety,” explains Samantha. “Over time, a person with anorexia will learn accidentally that if they starve themselves briefly, it sort of mimics what the hypothalamus would do under threat, which then lowers cytokines. And this makes them feel a little bit better, because the anxiety gets reduced.”
Unfortunately, the body soon becomes used to this trick. ”The body goes, ‘Oh, okay, we're not going to eat so much now, but the perceived threat remains.’ So even though you’re eating less, the cytokines continue to rise. To feel the same reduction in anxiety, you have to starve yourself more and more. So by the time you get down to the bottom of this spiral, you've lost a whole lot of weight.”
How Boswellia might help break the anorexia spiral
Boswellia – known for its anti-inflammatory properties – might be able to interrupt this dangerous spiral through its ability to cross the blood-brain barrier and reduce neuroinflammation, by inhibiting the production of cytokines.
One of the main active compounds in Boswellia, AKBA, may do this by blocking a protein that triggers the body’s inflammatory response.
Samantha and her team at Liverpool John Moores University are putting this idea to the test with a small clinical study exploring whether Boswellia can help people with anorexia nervosa by calming inflammation in the brain.
“What we're saying is: rather than use appetite restraint to lower your cytokines, use Boswellia to lower your cytokines,” says Samantha. “Obviously, it’s only one part of the problem, because we need to address the thing that elevates the cytokines in the first place.”
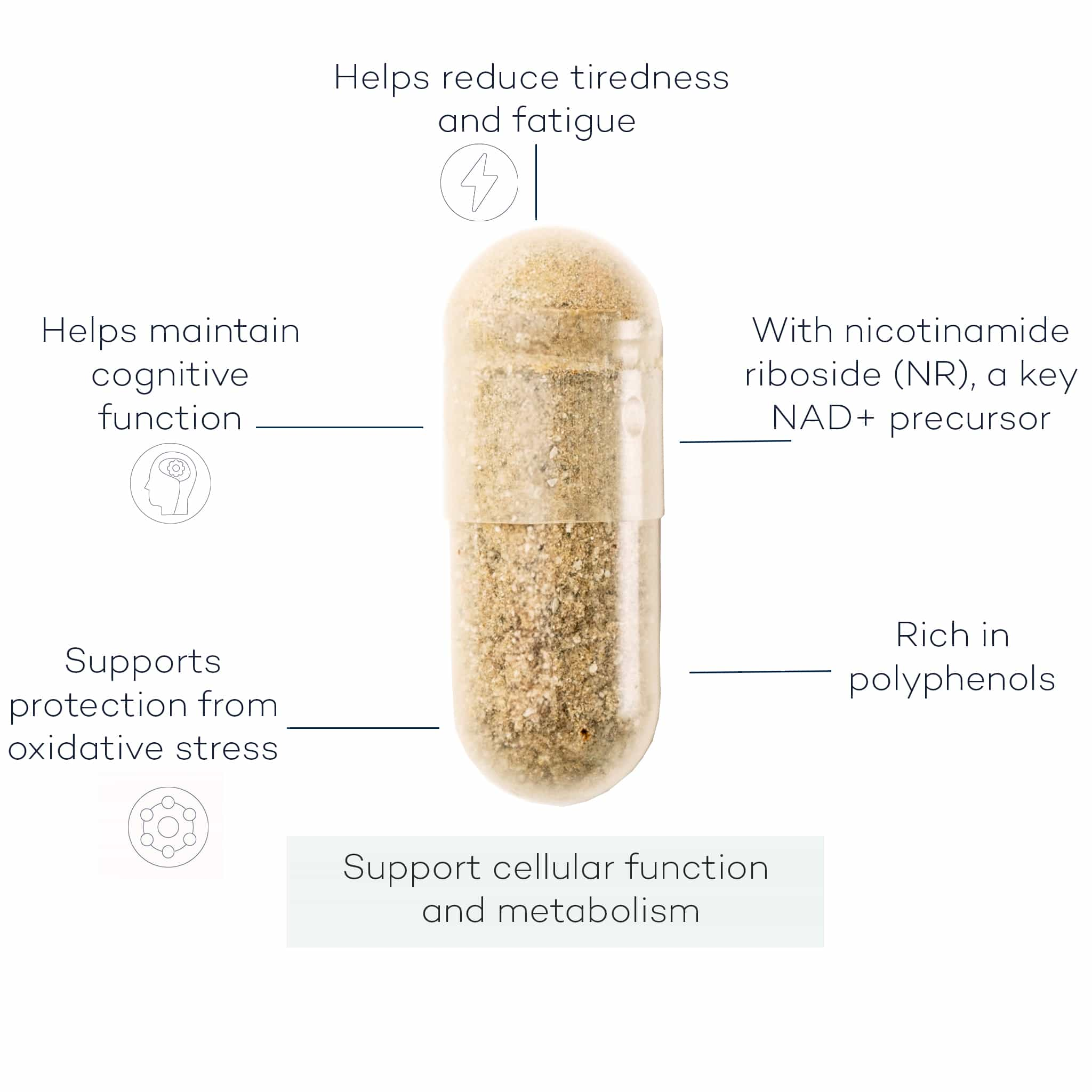
In the study, participants diagnosed with anorexia will receive either daily Boswellia in the form of a Cool Joints+ capsule, or a placebo, alongside a healthy control group.
By reducing cytokine activity, Samantha hopes to ease the neuroinflammatory processes that drive anxiety and compulsive food restriction – and, ultimately, open up new treatments beyond traditional psychotherapy.
“We need many more longitudinal studies to see if it works, and taking a pill is not a catch-all solution,” cautions Samantha. “But I do believe that if you have therapy alongside a daily anti-inflammatory supplement and a good diet of fruit and veg, that will improve your cognitions and help you.”
Dr Miriam Ferrer, PhD, the Head of Product Development at FutureYou Cambridge, says: “We’re honoured that our Cool Joints+ formulation is part of this pioneering research. It’s inspiring to see high-quality nutritional science being applied in such an important area of mental health, and we’re looking forward to discovering more about how Boswellia might offer support to people with eating disorders.”
References
Brooks, J Mol Targeting Cytokines in the 5-LOX Pro-Inflammatory Pathway for Treatment-Resistant Anorexia Nervosa Genet Med 2018, 12:4
Brooks SJ, Dahl K, Dudley-Jones R, Schiöth HB. A neuroinflammatory compulsivity model of anorexia nervosa (NICAN). Neurosci Biobehav Rev. 2024;159:105580.
Disclaimer: Please note that FutureYou Cambridge does not sell products designed to treat eating disorders. If you need support, please contact your healthcare provider.









Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.